What is the development of artificial joints?
Introduction:With the rapid development of material science, bioengineering and surgical technology, artificial joints have evolved from simple substitutes to highly precise and biocompatible bionic devices. They can not only effectively relieve pain and restore joint function, but also greatly improve patients’ mobility and quality of life. From the replacement of hip, knee, shoulder and even smaller joints such as knuckles, artificial joints are increasingly used in a wide range of applications, becoming an important means to treat severe arthritis, fracture failure, congenital malformations and other diseases. This article will delve into the history of artificial joints, material innovations, design concepts, surgical techniques, and their positive impact on patients’ lives, aiming to reveal the full picture of this medical miracle for readers.
History of prosthetic joint replacement
The history of artificial joint replacement can be traced back to the 19th century, and its development has experienced from the early exploration stage, gradual development stage to today’s more mature stage.
1. Early Exploration (early 19th century – late 19th century)
Early 19th century: The concept of artificial joint replacement begins to sprout. For example, in 1822, Dr. Anthony White of the United Kingdom performed a 5cm subtrochanteric osteotomy of the femur to improve hip function and relieve pain.
Mid-19th century: Initial attempts at artificial prosthesis replacement have been made. Between 1840 and 1860, JM.Carnochan in the United States first performed mandibular joint arthroplasty, using oak pieces as an implant, although the joint could move, but the oak pieces were later discharged causing the operation to fail, which is regarded as the beginning of artificial prosthesis replacement.
Late 19th century:Total hip replacement began to develop. In 1891, German doctor Gluck first used ivory femoral head and acetabulum to perform total hip replacement, and used bone glue as an adhesive to fix the prosthesis, which played an enlightenment role in the later application of bone cement type total hip replacement technology.
2.Gradual development stage (early 20th century – 1960s)
Early 20th century:Materials and techniques for artificial joint replacement are constantly improving. During this period, orthopedic surgeons tried a variety of different substances, from soft tissue to gold, in order to find suitable joint filling materials. These ideas were pioneering, but the results were not ideal. By 1923, American surgeon Smith Petersen devised glass arthroplasty, which is considered the originator of hip replacement.
Mid-20th century:With the continuous development of metal materials and biocompatible materials, the quality and effectiveness of artificial joints have been significantly improved. For example, in 1938, Smith Petersen found that the cobalt-chromium-molybdenum alloy used by dentists was more bioinert and biocompatible in the human body, so he made it into a metal cup with a bell opening for total hip replacement.
In the 1960s:The famous British joint surgeon S. J. Charnley (Sir John Charnley) proposed the low-friction artificial hip replacement theory in 1962, designed a 22.5mm diameter metal femoral head and ultra-high molecular polyethylene acetabulum combination prosthesis, fixed with polymethyl methacrylate (bone cement). Thus, low-friction artificial joint replacement was created.
3.Modern Maturity stage (1970s – present)
Since the 1970s: Due to the aging and fracture of the bone cement interface, prosthesis loosening and other complications, non-bone cement prosthesis has been rising again. At the same time, biological fixation methods have also begun to be explored and developed.
Since the beginning of the 21st century: in the application of artificial joint technology has entered the era of renovation. At the same time, the application of artificial joint replacement in elderly patients with osteoporotic femoral intertrochanteric fracture and femoral intertrochanteric fracture is becoming more and more widespread. In addition, joint replacements such as shoulder, elbow, and ankle joints are also being developed with good medium – and long-term results. With the advancement of biomaterials and surgical techniques, small joint replacement such as wrist joint, interphalangeal joint, metatarsophalangeal joint has been introduced one after another, bringing hope to patients with severe small joint diseases.
Artificial joint material type
Artificial joints are typically made from a variety of materials that are chosen to mimic the structure and function of the body’s natural joints while ensuring good biocompatibility, wear resistance and stability. The following materials are commonly used for artificial joints:


Artificial joints of different material
1.Metal alloy material
Metal materials have a wide range of applications in artificial joints and are favored for their high strength, wear resistance and good mechanical properties. Common metal materials include:
Stainless steel:Due to the high Cr content in steel, stainless steel materials have stronger resistance to a wide range of corrosive environments, it can form strong adhesion, with self-healing and corrosion resistant oxide coating Cr2O3. Stainless steel material has excellent processing performance and low price, which makes it widely used in the early days. However, its shortcomings are also obvious in later application: the prosthesis often has corrosion behavior and various failure forms in the body, and releases toxic ions due to wear, poor comprehensive tribological properties and other shortcomings, so it is now less used.
Cobalt-chrome-molybdenum alloy:Cobalt-chromium-molybdenum alloys have excellent corrosion and wear resistance. A passive oxide layer is formed on the surface of chrome-cobalt-molybdenum alloy to protect the internal material. Cobalt-chromium-molybdenum alloy is also insensitive to stress corrosion environments and has been used in the past as a material for joint replacement of metal hip prostheses. However, because this kind of alloy is in the erosion environment of human body fluids for a long time, and has to bear the weight and repeated friction, cobalt, chromium, molybdenum and other elements that are harmful to the human body are often inevitably released to the human body, resulting in poisoning, and such materials are poor in toughness, and the elastic modulus is far greater than the human bone. For safety reasons, the properties of such alloy materials need to be further improved.
Titanium alloy:Titanium corrosion resistance, high strength and good toughness, compared with other metal materials has good enough biocompatibility, is a better choice for artificial joint implants. In addition, titanium alloys also have other shortcomings: general friction and wear properties, elastic modulus does not match bone tissue, interference with MRI examination, and a small number of patients are allergic to it. Fortunately, there are more studies on titanium alloys, and in recent years, new β-titanium alloys have come out, and the elastic modulus of such titanium alloys is lower, the biocompatibility is better, and the overall development trend is good. Titanium alloy as artificial joint material market is large.
2.Organic polymer materials
Ultra-high molecular weight polyethylene (UHMWPE) : UHMWPE has high wear resistance and overall good biocompatibility. However, the residual free radical oxidation after friction will reduce the wear resistance, resulting in the formation of grinding chips, which will cause the body’s immune response, damage bone tissue and cause osteolysis. Therefore, the service life of artificial joint materials used alone is often not long. However, for a long time, a large number of domestic and foreign experts and scholars have studied the name change of UHMWPE, including radiation crosslinking, filling modification, surface modification and other methods to further improve the wear resistance of UHMWPE. However, due to the limitations of traditional UHMWPE materials, it is very difficult to improve its tribological and mechanical properties in a leap.
Carbon fiber reinforced polyether ether ketone (CF/PEEK) :Carbon fiber reinforced polyether ether ketone (CF/PEEK) : Polyether ether ketone (PEEK) is a thermoplastic special engineering plastic. Its excellent biomechanical and biotribological properties make it one of the research directions of artificial joint materials. PEEK material is a self-lubricating material, and its friction performance is even better than that of ultra-high molecular weight polyethylene. When it is used as a prosthesis material alone, its performance is poor. However, the friction and wear properties of polyether ether ketone materials after surface modification or composite materials composed of various polyether ether ketones are significantly improved. Carbon fiber reinforced technology is one of the most studied and effective means. PEEK has similar elastic modulus with bone, which brings significant advantages for PEEK in the medical field, especially as an implant material, such as reducing stress shielding effect, improving the binding effect of implants and bone, reducing the risk of secondary surgery, and promoting bone regeneration and integration. In this way, modified PEEK has great advantages as an artificial joint material, and more clinical research reports are expected.
3.Ceramic material
Ceramic materials are widely used in artificial joints because of their excellent hardness, wear resistance and biocompatibility. Common ceramic materials include:
Alumina ceramics: Because of its high hardness, good hydrophilicity, low friction coefficient, excellent physicochemical stability and biocompatibility, alumina ceramics have become one of the most common ceramic materials for the preparation of bioartificial joint materials. However, alumina ceramics also have obvious shortcomings, alumina ceramics are brittle, poor toughness, and the elastic modulus is much higher than that of human bone, easy to be subjected to uneven pressure distribution during human activities, and local pressure is too strong. The main research direction is to improve the poor frictional and mechanical properties of alumina ceramics by modification technology. However, it is undeniable that alumina ceramics have excellent wear resistance and broad application prospects.
Zirconia ceramics: ZrO2 ceramics have good properties, strength, toughness and other aspects are higher than Al2O3 ceramics, wear resistance is also better than Al2O3 ceramics, long service life, zirconia ceramics is considered to be the future of artificial joint implant prosthesis mainstream material. In terms of frictional properties, although the interface wear rate is low, the probability of fracture and abnormal sound of the prosthesis is far higher than that of other materials, which is determined by the high brittleness of the ceramic material itself and the poor bending resistance. There are relatively few studies on zirconia in the field of artificial joints, and there are not many cases of clinical use of zirconia ceramics, but in terms of frictional properties, such materials are better than the metal materials currently used.
The structure of artificial joint
An artificial joint is a medical device used to replace a damaged joint in the human body. For example, a hip and knee implant, as shown in the figure below, consists of the femoral shaft, the femoral head, the acetabulum cup (or acetabulum prosthesis), and may contain a acetabulum lining. These parts work together to mimic the function of a natural hip and help patients regain normal mobility and quality of life.
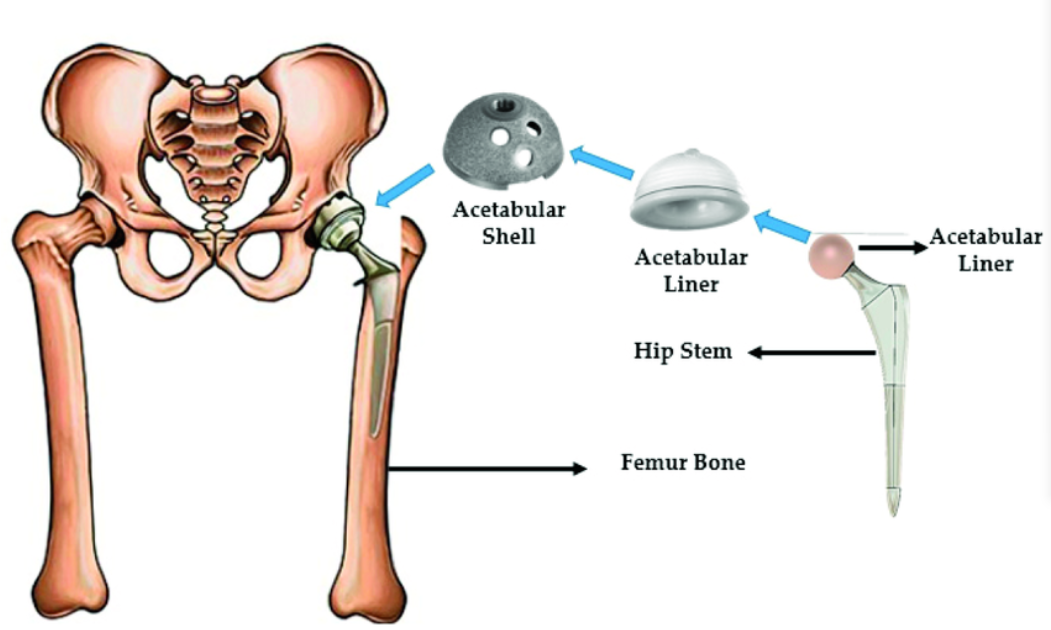
Femoral stalk:The femoral stem is an important component of hip implant prostheses that are inserted into a patient’s femoral canal to replace a diseased or damaged part of the femur.
Head of the thigh:The femoral head is another key part of the hip implant. It is attached to the top of the femur stem and is used to replace the removed femoral head. The femoral head is usually spherical in order to form a smooth friction interface with the acetabular lining.
Acetabular lining:The acetabular lining is an internal component of the acetabular cup that is in direct contact with the femoral head. The main function of the acetabular lining is to provide a smooth friction interface between the femoral head and reduce wear and friction generated debris.
Acetabular prosthesis:Acetabular prosthesis is the main part of hip implant prosthesis used to replace diseased or damaged acetabulum. The acetabular cup forms a joint with the femoral head, allowing normal flexion, extension, adduction, and abduction of the hip joint.
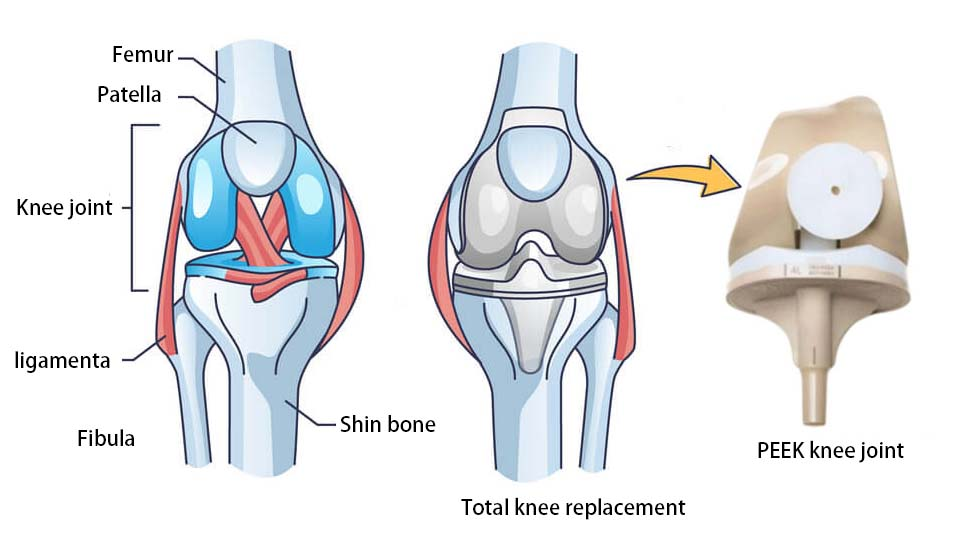
Femur prosthesis:A femur prosthesis is a part of an artificial knee joint that simulates the lower end of the femur bone. This part of the material needs to have good biocompatibility and enough strength to withstand the pressure brought by human activity and weight.
Patellar prosthesis:Patellar prosthetics are the same size as natural bone, slightly flat in shape and not completely round in shape. Patellar prosthetics are usually fixed to the original bone by special bone cement or screws. Patellar prosthesis plays an important role in restoring knee stability, alleviating knee pain, improving joint function and preventing further joint injury.
Shin gasket:Shin shims are cushioning parts that are placed between the shin rest and the femoral condyle and are usually made of a polymer material. This material has excellent wear resistance and lubricity, which can effectively reduce the friction between joint surfaces and improve the service life of joints.
Tibial prosthesis:Tibial prostheses are often designed to better match the shape and structure of the tibia, thus providing better support and stability. It may have a single prosthesis design or a two-part modular design, all designed to ensure that the prosthesis fits tightly into the tibia, reducing friction and wear while providing adequate support.
Artificial knee joint is a complex and fine medical device, its various components cooperate with each other to simulate the anatomy and function of the human knee joint to achieve the normal function of the joint. When choosing an artificial joint, the most suitable joint type and material should be selected according to the specific situation of the patient and the advice of the doctor.
Conclusion:Nowadays, with the cross-integration of multiple disciplines such as material science and bioengineering and the development of intelligent technology, joint replacement technology has shown a rapid development momentum. The development of new biocompatible materials, the improvement of personalized customization technology and the wide application of robot-assisted surgery systems will be the main driving force for the development of joint replacement technology. At the same time, with the aging of the population, the improvement of medical security policies and the growth of medical tourism and other factors, the artificial joint market will continue to grow and show a more diversified competitive pattern. In the future, artificial joint replacement will usher in a broader development prospect for more patients with joint diseases to bring better treatment results and quality of life.
